Table Of Contents
What Is A Bundled Payment?
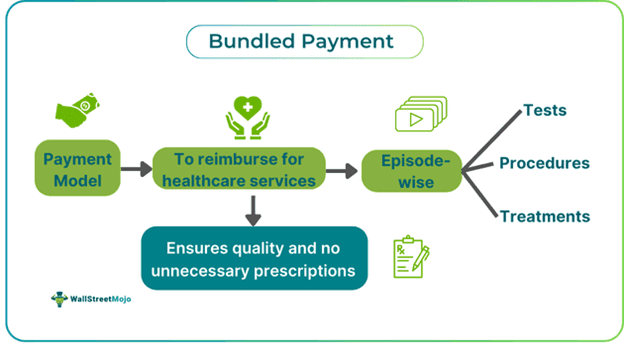
Bundled Payment is a model or system that facilitates one-time payment to those providing health care services. It eliminates care seekers’ pressure to pay, as providers receive the required predetermined payment until a certain limit is reached. This payment model improves healthcare quality, coordination, and cost efficiency.
You are free to use this image on your website, templates, etc.. Please provide us with an attribution link.
Medical checkups involve various treatments, procedures, and tests, and each step involves various costs to be paid at each stage of caregiving. Under this model, the payments are linked to care seekers, who are the beneficiaries in this case. The model encourages providers to offer quality services, incentivizing them to collaborate and deliver coordinated care.
Key Takeaways
- A bundled payment method consolidates healthcare payments into single sums for specific episodes of care provided by healthcare service providers.
- The strategies to ensure effective implementation include robust care coordination systems, multidisciplinary teams with designated Physician Champions, standardized care pathways, utilization of Electronic Health Records.
- It is vital for improving care coordination, containing costs, enhancing patient outcomes, fostering value-based care delivery, and aligning financial incentives with quality care.
- It differs from capitation and global payment methods in terms of structure and care coordination required or facilitated.
How Does A Bundled Payment Work?
Bundled payment in healthcare refers to the predetermined amount paid as reimbursement to healthcare service providers for particular episodes of care. An episode of care includes all sequential attention, treatments, and procedures given or carried out with respect to one’s single medical condition. It is a method of integrated payment a single time instead of paying separately for each service delivered.
This payment model is different from fee-for-service arrangements, where providers are reimbursed based on the volume of services rendered, which might increase expenses by promoting more tests and visits. Payment bundling, on the other hand, unites services for a certain episode of care, with authorities paying for the services based on the expected cost incurred all at once. If the providers can handle the episode of care within the budgeted amount, they can share the savings. This encourages providers to integrate care efficiently and discourages irrelevant services, hence increasing cost-effectiveness.
Bundled payment in healthcare might be limited to inpatient care or extended to encompass pre-operative treatment planning, outpatient treatments, and post-acute care. Negotiating bundling payments involves determining the services included in a bundle, which comprises three main components: service inclusion criteria, the period or the episode time window, and criteria for patient inclusion/exclusion.
- Service inclusion sets which services are necessary for specific episodes.
- The episode time window is tailored to each bundle type.
- Patient criteria, both inclusion and exclusion, are vital to checking patients' eligibility for the care they require compared to what providers usually offer.
Providers may be cautious about admitting patients with co-morbid conditions, even with risk adjustments, due to payment uncertainties. Payment rates, influenced by factors like risk adjustment or flat fees, determine bundle prices. Risk adjustment compensates for variations in patient care based on demographic and health factors (such as age). In such scenarios, flat fees offer a fixed rate per patient, often preferred for standardized care episodes.
Strategies
Some of the strategies adopted to give more clarity to the concept of bundle payment have been discussed in detail below:
#1 - Coordination
For any scheme to be effective and successful, it is essential that the parties involved in the process or planning coordinate well. The same applies to this concept of bundling payment. To enable this coordination, a tracking system is set up, which helps identify patients triggering episodes of care, ensuring timely interventions and follow-ups.
The model encourages the presence of a coordinator or nurse navigator who checks if the assigned duties to respective caregivers are being carried out properly. Conducting thorough initial assessments, possibly aided by risk assessment tools, allows care teams to tailor care plans to each patient's unique needs and preferences.
Collaboration among providers is essential for seamless patient care coordination and smooth transitions between different care settings. Establishing networks of high-quality post-acute care providers and collaboration among cross-providers also helps.
#2 - Implementation
The next on the list of strategies is to have a framework for the teams that would implement the bundled payment model. It includes building a diverse team of professionals and encouraging collaboration in delivering coordinated patient-centered care. Each team member brings unique expertise to contribute to comprehensive care delivery. Appointing a physician who is the most trusted engages fellow physicians in collaborative decision-making on clinical approaches. This individual promotes buy-in and support for care redesign processes among peers, enhancing overall implementation success.
Implementing care pathways or protocols standardizes care delivery for patients and care team members. These pathways outline standardized approaches from the beginning to the end of patient care, ensuring consistency and quality. A comprehensive education on targeted conditions and treatments ensures that all team members understand and comply with standardized care protocols. This enhances consistency and quality of care delivery across the organization.
The next step in deploying this strategy is to establish a rapid response team for high-risk clinical conditions to ensure swift and effective responses. This team adheres to predefined protocols on clinical approaches and patient-centered care, mitigating risks and improving patient outcomes.
#3 - Engagement
It is important to ensure caregivers and patients remain involved in utilizing this payment model. It enhances healthcare outcomes and fosters shared decision-making. Care teams prioritize understanding patients' needs and setting expectations early on to promote patient autonomy and choice. This facilitates the development of realistic care plans tailored to individual preferences, optimizing outcomes.
Educational materials are shared with patients and caregivers to facilitate informed discussions about care plans, procedures, and post-acute care. Providing resources in various formats and languages ensures accessibility and meets diverse preferences.
When the knowledge is sufficient, services become more easily accessible. Care team contact information is provided to improve patient access to care. This enables patients and caregivers to promptly access the necessary care and support when needed, promoting continuity of care.
#4 - Improvement
The next strategy that helps make this payment model reliable is the constant advancement it encourages. Authorities, like the Centers for Medicare & Medicaid Services (CMS) in the United States, deploy technological tools and techniques from time to time to ensure the model remains up to date.
Leveraging technology to streamline communication among care team members requires focus. It also enables direct communication of care coordination needs with patients and caregivers.
In addition, Electronic Health Record (EHR) systems with alerts notify team members of specific criteria or needs, facilitating timely interventions and adherence to care protocols.
Examples
Let us look into a few instances to understand the bundled payment definition better:
Example #1
Suppose Hospital ABC, a newly built facility, is implementing bundled payment models to improve patient-centered care and cost-effectiveness. The process is followed to set it up included the following steps:
- They identified specific clinical episodes where bundled payments could be effective, such as joint replacement surgeries.
- They collaborated with orthopedic surgeons, anesthesiologists, physical therapists, and post-acute care providers to develop a comprehensive care pathway.
- The framework was set up, which included pre-operative consultations, surgical procedures, hospitalization, rehabilitation, and post-discharge follow-up.
- The financial arrangements provided a single, fixed payment for the entire episode of care, incentivizing efficient resource utilization and coordinated care delivery.
- The hospital invested in robust care coordination tools, electronic health recording systems, and data analytics capacities to ensure successful adoption.
The bundled payment implementation aimed to improve care coordination, reduce readmissions, and enhance patient satisfaction. They actively engaged patients in shared decision-making, providing education and support throughout the care journey to optimize outcomes and minimize complications. As a result, Hospital ABC experienced positive outcomes, including reduced hospital stay length, improved patient experiences, and better cost management.
Example #2
An April 2020 study conducted by the Commonwealth Fund evaluated the empirical evidence regarding their influence on healthcare quality and expenditure. The researchers examined 23 initiatives in eight countries, focusing on bundled payment models adopted for various procedures and chronic conditions. Out of 35 studies analyzed, most indicated positive effects on the quality of health care and medical spending. Specifically, 20 studies demonstrated modest savings or reduced spending growth, and 18 reported enhancements in quality measures.
The study used as an example shows how these payment models exhibit the potential to mitigate the growth of medical spending while either positively impacting or maintaining the quality of care. The study also highlights the overall efficacy of the payment models in achieving their dual objectives across diverse healthcare settings and conditions.
Importance
The importance of such payment system lies in its capacity to:
- Improve healthcare coordination and collaboration among healthcare providers
- Drive cost containment by reducing unnecessary utilization of resources
- Enhance patient outcomes and satisfaction through coordinated care efforts
- Foster value-based care delivery and continuous quality improvement initiatives
- Align financial incentives with the achievement of better patient outcomes and the delivery of cost-effective care
Bundled Payment vs Capitation vs Global Payment
The differences between the concepts are given as follows:
Definition
Bundled payment centers on a distinct care episode, capitation offers a set payment per patient within a set timeframe, and global payment encompasses all healthcare services for a defined population.
Payment structure
Bundled payment consolidates payments for various services into one, capitation supplies a fixed payment per patient, and global payment offers a lump sum covering all services.
Care coordination
Bundled payment drives care coordination for specific episodes. Capitation emphasizes primary care and preventive services, and global payment fosters population health management.